Novel Imaging Technology Reveals Role of Immune Cells in Early Diabetic Cataract Development
Diabetic complications may start during the pre-diabetic state
Novel findings from researchers at the Brigham and Women's Hospital and Harvard Medical School, in collaboration with the Health Campus Göttingen contradict previous notions about sugar's role in the onset of diabetic cataracts. The team of researchers, led by Prof. Dr. Ali Hafezi-Moghadam, Director of the Molecular Biomarkers Nano-Imaging Laboratory (MBNI), in collaboration with Professor Dr. Christoph Rußmann, Dean of the Health Campus and a Visiting Professor at MBNI, found early signs of damage in the eye before the onset of type 2 diabetes, suggesting that diabetic complications may start during the pre-diabetic state. The team has published the results in the Journal of Biomedical Science.
Cataracts — the clouding of the lens of the eye — are the number one cause of blindness worldwide and are a common complication of type 2 diabetes. The current hypothesis behind cataract development is coined "the sugar hypothesis" and suggests that high blood sugar — a hallmark of diabetes — precedes cataract development. The working assumption underlying the sugar hypothesis describes that higher levels of glucose in the lenses of individuals with diabetes converts to a sugar alcohol molecule called sorbitol, which induces structural changes to the lens of the eye that precede cataract development. While unproven, researchers rarely investigate this theory further due to cataracts' treatable nature. “A theory can survive for a long time, if it is unchallenged” said Hafezi-Moghadam.
“For over half a century, the sugar hypothesis provided an explanation for how the lens becomes opaque, when the blood sugar in an animal is experimentally raised." said Hafezi-Moghadam, "but this does not have to be how things work in human cataracts.”
To unravel the origins of tissue damage in diabetes, Hafezi-Moghadam’s team broke tradition with the existing models. Instead, it conducted it’s studies in the Nile grass rat, a model that they originally reported spontaneously develops type 2 diabetes when kept in captivity and closely mimics the condition in humans. In addition, “the advanced imaging technology we used in this study” said Rußmann “helped us see for the first time dot-like microlesions that would not have been visible otherwise. This is where advanced medical technology helps bring novel mechanistic insights.”
The newly found micro-lesions preceded all forms of diabetic cataract. But unexpectedly in nearly half of the animals, the micro-lesions appeared before the animals entered hyperglycemia, or high blood sugar. “It became clear that there was more complexity than the sugar hypothesis was able to explain” said Dr. Ehsan Ranaei Pirmaradan, the first author of the study and a postdoctoral fellow at MBNI and Harvard Medical School. “We found immune cells in the vicinity of the lens and in the lens capsule. That drew our focus to a completely new direction.”
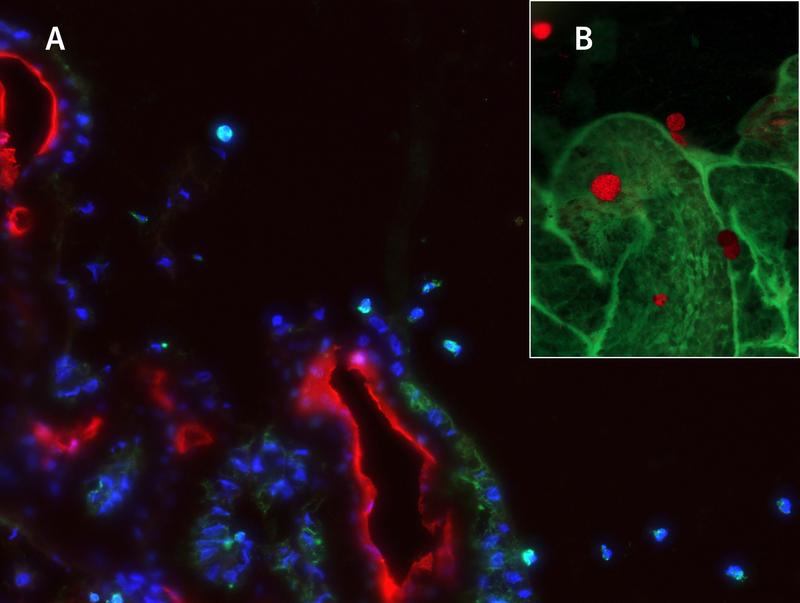
The researchers identified that immune cells migrated from specialized structures in the eye called the ciliary bodies toward the lens. In these areas, where the immune cells traversed the capsule of the lens, they found that the epithelial cells that normally cover the inner surface of the lens capsule changed their identity and behaved differently. These changes, also referred to as epithelial-mesenchymal transformation (EMT), were followed by seemingly unorganized cell growth, cell death, and cell migrations into the body of the lens. In some regions, the newly transformed cells simply vacated their original positions and made their way into the lens. Such cellular changes, however small in dimensions, significantly compromise the function of the lens. “It was fortuitous that our imaging technology had just high enough resolution to see such microscopic lesions in the living organism.” said Rußmann “A future direction will be to turn this knowledge into early clinical diagnosis.”
“Our study raises exciting new questions, which will preoccupy us in the foreseeable future” said Hafezi-Moghadam “We need to understand why the immune cells and the lens epithelial cells behave the way they do before the blood glucose becomes higher than normal. This will bring us closer to understanding why diabetic complications may start during the pre-diabetic stage of the disease.” With such knowledge, Hafezi-Moghadam envisions, “we can start to search for how to prevent people with diabetes from developing cataracts and potentially other complications elsewhere in the body.”
“While cataracts today are easily removable with surgery, this procedure comes with the risk of complications” said Hafezi-Moghadam. “With over 500 million people worldwide having diabetes, there is an urgent need for trying to find non-surgical ways of preventing, slowing, or even reversing this complication. Perhaps one day it will become possible to avoid performing these surgeries altogether. And that requires that we return to the basics.”
HAWK's Prof. Rußmann has been a long-term collaborator of Prof. Hafezi-Moghadam at Harvard. The investigators have recently been awarded an international grant through the US National Science Foundation (NSF) and the Federal Ministry of Education and Research in Germany to deepen their transatlantic collaborations. “You need the most innovative technologies applied to the best-existing animal models to address the urgent medical needs of our time,” states Hafezi-Moghadam “and sometimes it leads to novel insights that help forming a new paradigm.”
Funding: This work was supported by NIH Impact Award (DK108238-01, AHM), and JDRF Innovation Award (INO-2016-222-A-N, AHM).
The Health Campus Göttingen is a collaboration between the University Medical Center Göttingen and the HAWK University of Applied Sciences and Arts Hildesheim/Holzminden/Göttingen.
Some statements int this press release are based on a prior press release by BWH, a founding member of Mass General Brigham.
Download article
Reference:
Hafezi-Moghadam et al. “Pre-hyperglycemia immune cell trafficking underlies subclinical diabetic cataractogenesis.” Journal of Biomedical Science 30, 6 (2023). https://doi.org/10.1186/s12929-023-00895-6.
Caption:
Immune cell trafficking in diabetic cataract formation. (A) Immune cell passing through ciliary body’s epithelial cells. (B) Attached immune cells (red) on the ciliary body (green) in a flatmount preparation.
Sabine zu Klampen
Press Officer
HAWK
University of Applied Sciences and Arts Hildesheim/Holzminden/Göttingen
Public Relations Office
Hohnsen 4, Room 105 | 31134 Hildesheim, NI
Germany
E-mail: sabine.klampen@hawk.de
Tel.: 00495121/881-124
Fax: 00495121/881-200124
Mobil: 0049163/586676 3
www.hawk.de
UNIVERSITY MEDICAL CENTER GÖTTINGEN
GEORG-AUGUST-UNIVERSITÄT
Corporate communication
Public relations
Von-Siebold-Str. 3, 4th Floor, Annex A
37075 Göttingen, NI
Germany
Mail address: 37099 Göttingen
Germany
Telephone 0049551 / 39-61020
Fax 0049551 / 39-61023
www.umg.eu
Wissenschaftlicher Ansprechpartner:
Ali Hafezi-Moghadam, MD, PhD
Director of the Molecular Biomarkers Nano-Imaging Laboratory (MBNI)
Molecular Biomarkers Nano-Imaging Laboratory (MBNI), Brigham and Women’s Hospital, and Department of Radiology, Harvard Medical School, 75 Francis St., Thorn Research Building, Boston, MA, 02115, USA
E-mail: ahm@bwh.harvard.edu
Prof. Dr. rer. nat. Christoph Rußmann
Dean of the Health Campus Göttingen
Annastraße 25 (Room GÖO_209)
37075 Göttingen, NI
Germany
E-mail: christoph.russmann@hawk.de
Tel.: 0049551/3705-217
Originalpublikation:
Hafezi-Moghadam et al. “Pre-hyperglycemia immune cell trafficking underlies subclinical diabetic cataractogenesis.” Journal of Biomedical Science 30, 6 (2023). https://doi.org/10.1186/s12929-023-00895-6.
Weitere Informationen:
https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-023-00895-6
Die semantisch ähnlichsten Pressemitteilungen im idw