Safe journey into the heart
Hereon sensors facilitate minimally invasive surgery for atrial fibrillation in heart patients
Atrial fibrillation can cause dangerous blood clots to form in the heart. Many patients therefore have the part of the heart where the clots form closed off with a plug. However, these so-called occluders do not always seal perfectly, which can lead to complications. The Helmholtz-Zentrum Hereon at its Teltow site is developing an occluder with sensors that can be placed precisely in the heart. The GoBio Initial funding of the Bundesministerium für Bildung und Forschung (BMBF) will bring the project to the next level towards clinical applications.
Around 60 million people worldwide are affected by atrial fibrillation. This form of cardiac arrhythmia means that parts of the heart, the atria, no longer contract properly, but instead move quickly and disorderly. This significantly disrupts the flow of blood through the heart. Especially at the small protrusions of the left atrium, the so-called left atrial appendage, the blood flows turbulently and almost chaotically. This can cause blood clots to form, clogging the arteries and leading to a stroke.
Many people affected by atrial fibrillation therefore receive small plugs that are implanted in their hearts - an established procedure. These “occluders” seal off the appendage of the heart so that blood can no longer flow into it. This works well for some patients. The occluders fit perfectly. This also reduces the risk of blood clots forming. In some patients, however, the occluders do not seal properly. Small gaps remain between the occluder and the inner heart tissue, through which the blood can flow in and out again. Blood clots can form despite the occluder. The surgical procedure was in vain.
A perfect fit
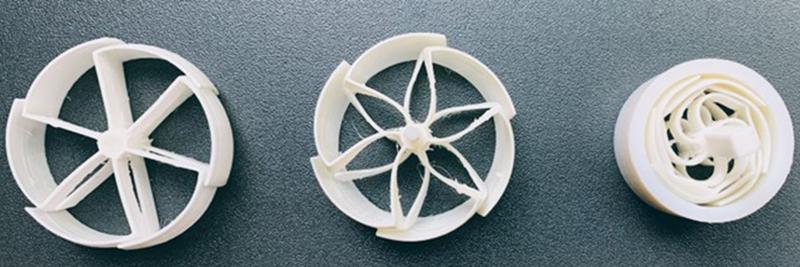
A research team from the Hereon Institute of Active Polymers in Teltow therefore teamed up with doctors from the Charité Hospital in Berlin some time ago to develop occluders that can be inserted more precisely into the left atrial appendage of the heart. These are better than traditional plugs in several respects. Until now, commercially available occluders have only been available in standard sizes with fixed diameters. As a result, they do not always fit perfectly. The occluders developed by the research team can be widened and closed in a similar way to the aperture of a camera - and can therefore be positioned much better in the opening of the appendage.
“The advantage of our collaboration is that doctors and material scientists work closely together here,” says Teltow scientist Dr Katarzyna Polak-Kraśna, who heads the Digital Design and Processing department. “We are working with interventional cardiologist Dr Markus Reintaler from Charité, who has a lot of experience with such operations.” Today, occluders are inserted minimally invasively into the heart via catheters - i.e. pushed through large blood vessels into the atrium. One challenge for the doctors is that they cannot really observe from the outside whether the occluder is well positioned. The position can only be corrected using imaging techniques such as X-ray or ultrasound. Small gaps between the occluder and the appendage can hardly be detected. The new occluders therefore include a second special feature. Wafer-thin sensors are attached to their surface, which can sense whether the occluder is firmly in contact with the tissue or not.
Nanometer-fine surface structure
The production of such special surfaces - so-called active polymer surfaces - is a core competence of the Hereon team. For the occluders, a wafer-thin fabric is first produced from nanometer polymer fibres. To do this, a liquid polymer is chased through a nozzle, from which the fibers shoot out like the thread of a spider. These fibers are then laid on top of each other in a criss-cross pattern until a fabric is produced that resembles the fine tangle of fibers of a Kleenex tissue under the microscope. This process is called electrospinning. In a second step, the sensors are integrated onto the fabric. The fabric is then bonded onto the occluder.
After two years of work, the first prototypes have been created. The project has now received over one Million Euros in funding within the GoBio Initial program, run by the Bundesministerium für Bildung und Foschung (BMBF), for a further two years. This means that the occluders in the initial preclinical phase will be tested in real pigs’ hearts from next year. “That will be exciting, because it will show how well the occluders work in the living, moving heart,” says Katarzyna Polak-Kraśna.
After successful first-in-animal tests, the team is planning a spin-off, that will allow bringing the device into clinical trials and to the clinics, to improve procedural outcomes of patients and decrease their risk of stroke.
Wissenschaftlicher Ansprechpartner:
Dr Katarzyna Polak-Kraśna I Helmholtz-Zentrum Hereon I Institute of Active Polymers in Teltow
T: +49 (0) 3328 352-303 I Katarzyna.Polak-Krasna@hereon.de I www.hereon.de
Ähnliche Pressemitteilungen im idw