Towards understanding inflammation in depression
Roughly one third of patients with depressive symptoms have elevated levels of inflammation. Inflammation is however often only measured using very broad and unspecific markers. To better understand the connection between depression and the immune system, researchers at the Max Planck Institute of Psychiatry measured a large amount of different biological factors and identified patterns in the data.
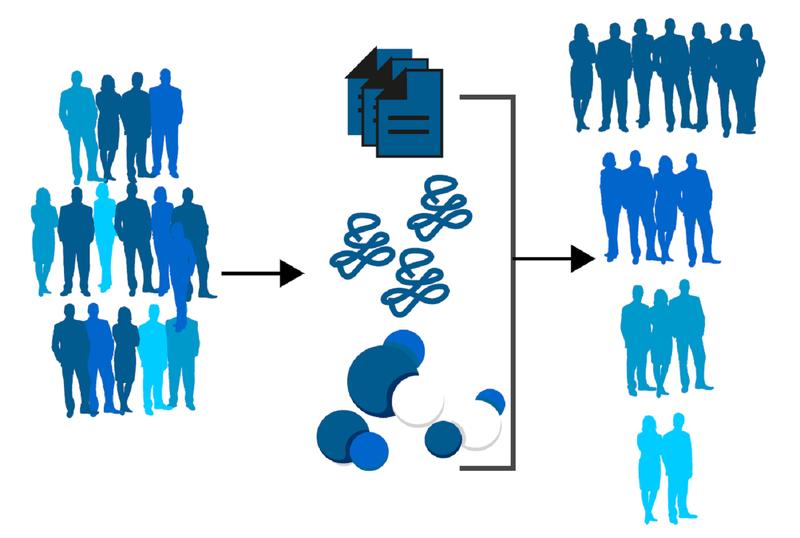
In the newly published study, first author Jonas Hagenberg and scientists from the Project Group Medical Genomics, led by Janine Knauer-Arloth, measured over 40 immune markers in the blood of 237 participants. This was a transdiagnostic study, meaning that researchers did not just include participants affected by depression, but also those with other disorders such as anxiety or substance use. In addition to immune markers, the scientists measured the activity of over 12.000 different genes in immune cells, as well as depressive symptom load. They also included body mass index (BMI) and the age of the participants, since both these factors impact inflammation. Using machine learning methods, the researchers then tried to recognize patterns in the data.
The team identified four different participant clusters. Besides CRP, the standard marker used to measure inflammation, the immune markers IL-1RA, TNF-alpha and several chemokines were helpful in defining these clusters. Chemokines are a specific class of immune markers. 121 participants fell into the largest cluster – these patients had fewer depressive symptoms, low levels of inflammation, and tended to be younger. The two next clusters consisted of 77 participants total, characterized by high depressive symptom load, high levels of inflammation, and an increased BMI. The final cluster consisted of 39 participants who displayed a high depressive symptom load but low levels of inflammation.
Gene activity levels mainly differed between the cluster that contained patients with fewer symptoms and the remaining three clusters, where patients had more symptoms. Interestingly, the analysis showed that some of the genes associated with depression were connected to specific immune cells, suggesting that certain types of immune cells may be more relevant in depression than others.
“Our results show us that while CRP is a good marker, there are also others that might be useful and that warrant further research – such as IL-1RA and chemokines”, Hagenberg explains. “Additionally, the connection between depressive symptom load, inflammation markers and BMI shows that depression needs to be treated holistically – this is not a new finding, but it underlines the importance of body weight”.
Including data beyond CRP provides researchers with a deeper understanding of the connection between the immune system and depression. These insights can help to develop more individualized and precise treatments for sub-groups of depressive patients in the future.
Wissenschaftlicher Ansprechpartner:
Jonas Hagenberg (jonas_hagenberg@psych.mpg.de)
Originalpublikation:
Hagenberg et al., Dissecting depression symptoms: Multi-omics clustering uncovers immune-related subgroups and cell-type specific dysregulation, Brain, Behavior and Immunity (2025), https://doi.org/10.1016/j.bbi.2024.09.013
Ähnliche Pressemitteilungen im idw